As a scientist who also suffers from vitiligo, I spent a day trying to read the current SCIENTIFIC findings published in peer-reviewed scientific journals.
- Two type of vitiligo: segmental (localized) vs. non-segmental. Most are non-segmental.
- Some evidence suggests that vitiligo patients are low in antioxidants, vitamin D, zinc, and copper. Vitiligo patients often suffer low glutathione peroxidase (GPx) as suggested by this and other papers.
- Vitiligo is a loss of pigmentation in the skin. Loss of a type of cells called melanocyte that produces melanin. Pathology is unclear, but the evidence is strong for autoimmune disease. In other words, our immune cells attack melanocytes. Oxidative stress by reactive oxygen species might play a role.
- There is no cure for vitiligo. But most patients see improvements with current treatments. It may take months.
- Many treatment exits, but few are rigorously tested in controlled clinical trials. Scientifically sound results published in peer-reviewed scientific journals are available in PubMed.org.
- Standard treatment protocols recommended by scientists and doctors, such as the Vitiligo European Task Force. The following charts are from a book “Pigmentary Disorders: A Comprehensive Compendium” by Koushik Lahiri, Manas Chatterjee, Rashmi Sarka.
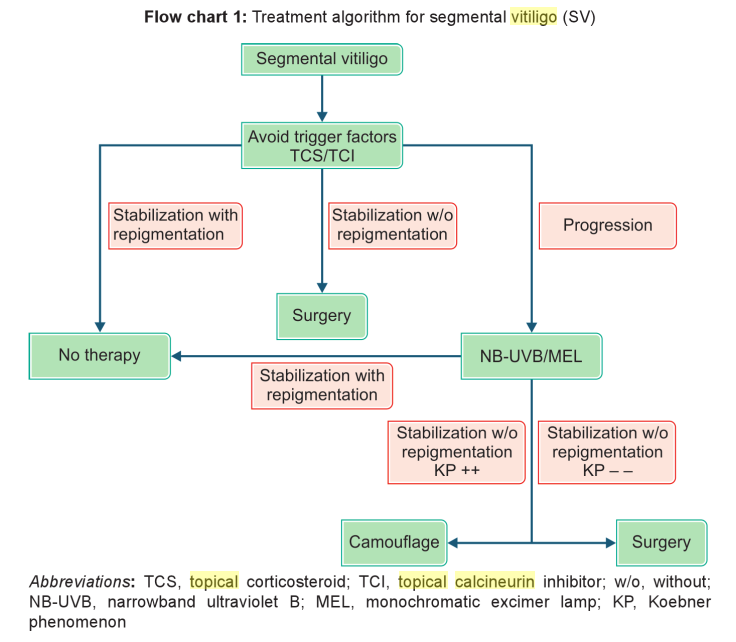
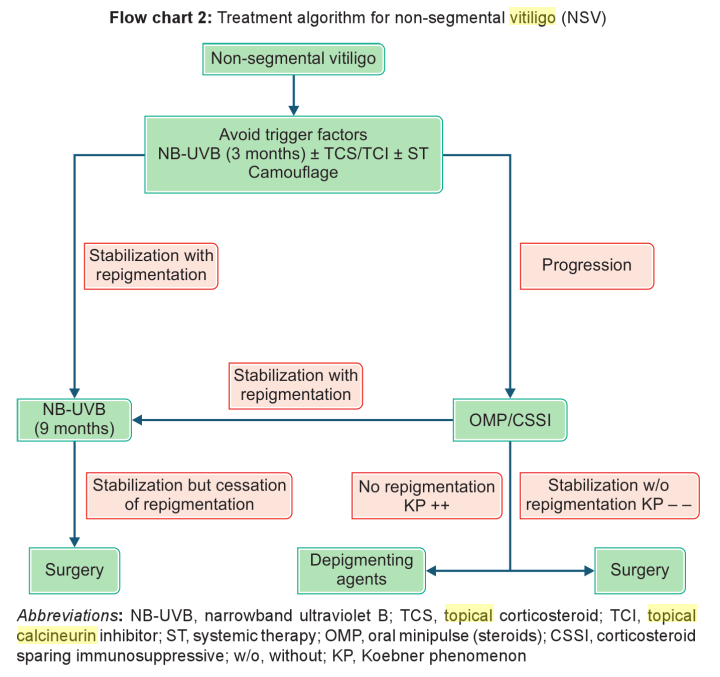
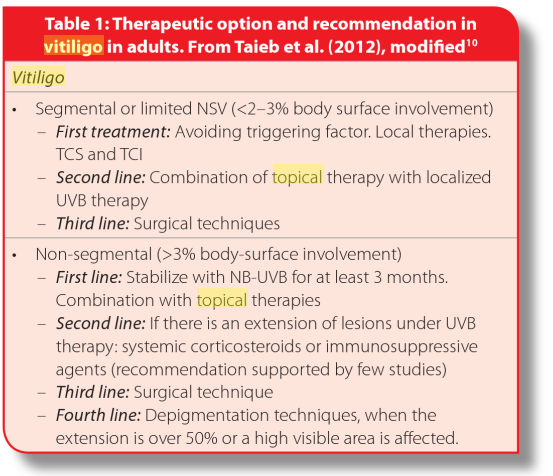
As can be seen from these two figures, the most widely used therapies are Narrow-band ultraviolet B (NB-UVB), topical corticosteroid, topical calcineurin inhibitors. These therapies can be classified into the following categories:
- Phototherapy uses different lights to treat vitiligo. Narrow-band ultraviolet B (NB-UVB) is one of the most effective methods. It can be targeted to small areas or the whole body.
- Topical therapies such as a topical corticosteroid, topical calcineurin inhibitors (Tacrolimus, pimecrolimus, etc.) are effective for selected areas. But not for long-term use. These are standard recommended methods to try first for segmental vitiligo, small, limited patches. For large areas of vitiligo throughout the body, the standard approach is NB-UVB for three months, in combination with topical therapies.
- Systemic treatment can be done through oral medicines such as corticosteroids. Oral corticosteroids are shown to stop the progression of vitiligo and induce repigmentation. But side effects are a concern. Antioxidants, either oral or topical, can help protect against reactive oxygen species that are believed to cause vitiligo.
- Surgical therapy. Transplant of skins or even hair follicular. Methods such as suction blister epidermal grafts are very effective and safe.
- Camouflage. Cosmetic camouflage improves quality of life. Some are permanent (tattoos, and micropigmentation) should be used with caution. Using DHA creams to camouflage seem to be safe and effective. These creams are used in self-tanning and will last 5-7 days.
- Combination therapy combines these methods.
- Topical creams are often combined with phototherapy.
- Oral MPD mini-pulse therapy combined with NBUVB appears effective in arresting vitiligo progression and rapidly inducing repigmentation with minimal side effects.
- The combined treatment with oral ALA, betamethasone injection and NB-UVB was effective and safe on non-segmental progressive vitiligo. ALA could accelerate the initial response of repigmentation.
- Alternative therapy. Many are being tested. But their effectiveness are not well supported.
- Diet supplements such as Vitamin C, E, ginko biloba extracts. Supplements for zinc and copper. L-phenylalanine used with phototherapy, and oral Ginkgo biloba as monotherapy show promise.
- Some Chinese herbal medicines act as photosensitizing agents to induce effects like sun burn to treat vitiligo.
- Combine vitamin E with phototherapy.
My vitiligo, however, keeps progressing. Hope someday there is a safe and effective cure.